Personalized Treatment Focusing on Lifestyle Factors May Lower Risk of Atrial Fibrillation
Atrial fibrillation (AFib), a common type of arrhythmia, comes with a global prevalence over [relevant data]. Beyond obvious risk factors connected to cardiovascular health, this condition is also associated with diabetes, obesity, smoking, and a host of chronic conditions such as cardiovascular, respiratory, metabolic, and mental health issues.
According to research, lifestyle factors, comorbid conditions, and socioeconomic status can all influence the risk of AFib. Physical activity, as part of a balanced lifestyle, is key to reducing AFib risk. Daily exercise, including high-intensity interval training, is beneficial for improving quality of life in individuals with AFib. Though studies show a connection between physical activity and reduced heart failure and cardiovascular-related mortality, the evidence pointing towards stroke prevention is less conclusive.
Obesity is another risk factor for AFib, increasing the likelihood of complications and recurrence. Weight loss can help minimize the risk. While there's ongoing debate about moderate-to-heavy alcohol consumption's connection with AFib, excess drinking is generally considered harmful. Interestingly, the involvement of smoking in AFib risk appears in a dose-dependent manner.
Chronic health conditions, such as obstructive sleep apnea (OSA), cardiovascular disease, and diabetes, also play a crucial role in AFib development and complications. OSA can lead to changes in heart structure and increased blood clot formation. Utilizing a continuous positive airway pressure (CPAP) machine for OSA management can help decrease AFib risk. Efficient management of comorbid conditions, like hypertension, can lower the chance of AFib complications, such as stroke.
Lifestyle adjustments, medication, and, in some cases, invasive procedures like catheter ablation, serve as AFib management strategies. Blood thinners or anticoagulants help inhibit blood clot formation and reduce stroke risk. After the introduction of nonvitamin K antagonist oral anticoagulants (NOACs), they've become the preferred initial treatment for AFib. Drugs like beta-blockers and calcium channel blockers are useful in controlling heart rate.
Other lifestyle factors contributing to AFib risk include inadequate sleep, high stress levels, and depression. Although the connection between mental health conditions and AFib isn't entirely understood, it's suggested that mental health issues could impact adherence to medications and potentially increase the risk of interactions between drugs used for AFib and mental health disorders.
When managing AFib, it's essential to adopt a personalized approach tailored to each patient's unique risk factors. A multidisciplinary team is best-suited to provide comprehensive care that addresses various factors influencing AFib, such as lifestyle choices, genetics, and socioeconomic standing. Patients with multiple chronic health conditions face an increased risk of complications due to increased medication use and potential drug interactions.
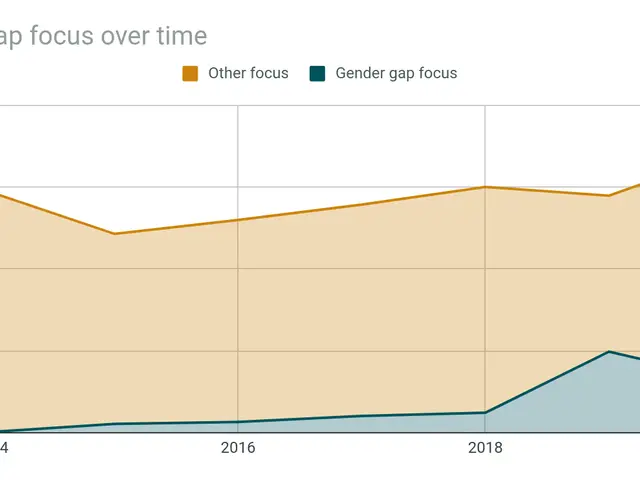
There's ongoing research on the role of ethnicity and sex in AFib development. Some studies have shown women to be more susceptible to complications, including stroke and mortality, while men are generally more affected by AFib. Access to healthcare and psychological factors such as stress may contribute to these disparities.
In summary, understanding the relationship between lifestyle factors, comorbid conditions, and AFib is crucial for effective management. By adopting a tailor-made approach involving healthy lifestyle choices, managing comorbid conditions, and seeking personalized medical care, individuals can significantly reduce their AFib risk and improve their quality of life.
- Atrial fibrillation (AFib) is connected with diabetes, obesity, smoking, and a range of chronic conditions, including cardiovascular, respiratory, metabolic, and mental health issues.
- Physical activity, part of a balanced lifestyle, plays a vital role in reducing the risk of AFib.
- Studies suggest that high-intensity interval training and daily exercise can improve the quality of life for individuals with AFib, though evidence for stroke prevention is less definitive.
- Obesity increases the risk of AFib complications and recurrence, making weight loss a helpful strategy.
- Chronic health conditions, such as obstructive sleep apnea (OSA), cardiovascular disease, and diabetes, significantly impact AFib development and related complications.
- Utilizing a continuous positive airway pressure (CPAP) machine for OSA management can help decrease the risk of AFib.
- Blood thinners or anticoagulants can inhibit blood clot formation and reduce stroke risk, while drugs like beta-blockers and calcium channel blockers are useful in controlling heart rate.
- Mental health conditions, such as depression, inadequate sleep, and high stress levels, could potentially increase the risk of AFib and impact adherence to medications.
- Adopting a personalized approach, tailored to each patient's unique risk factors, and seeking comprehensive care from a multidisciplinary team can significantly reduce the risk of AFib and improve quality of life for those affected.